Research Spurred by Tulane Economists Leads to Covid Study
Originally published in the Summer 2022 School of Liberal Arts Magazine
Monday, August 15th, 2022
Dean Brian Edwards sits down with three Tulane scholars—two economists and a public health expert—who recently co-authored a study investigating the effects of Covid-19 school closures on public health outcomes, to discuss what can be gained from collaborating across disciplinary lines. Their paper received national press attention and was cited by the CDC. But Edwards was most interested in their process itself.
Douglas N. Harris Chair and Professor, Department of Economics, School of Liberal Arts

Engy Ziedan Assistant Professor, Department of Economics, School of Liberal Arts

Susan Hassig Director, MPH Program in Epidemiology, School of Public Health & Tropical Medicine
Brian Edwards (BE): I believe that collaboration is a key value of a liberal arts education. How do you think about working with other scholars in academia, which so values individual accomplishment?
Douglas N. Harris (DH): I don’t think we really asked that question. I don’t see that as a tension, necessarily, that we’re going to somehow lose credit if we collaborate, or it’s going to be seen as strange. I tend to think about problems and questions I want to address, and then determine what is needed to tackle that problem or answer that question. That process is what brought the three of us together on this project. We saw a problem that we wanted to address.
BE: Your take is, in a way, a bit radical. Many have critiqued contemporary America for being hooked on the idea of individual achievement— that we’re obsessed with it. How did your group manage the impulse for sole credit?
DH: I agree. I don’t think others necessarily think the way I do. It’s different when you don’t have tenure, because you need to think about it in terms of how you’re going to be evaluated. In the tenure process, the department needs to determine your intellectual contribution and, as an element of understanding, your contribution and future standing in the field.
BE: Engy, as a younger economist working to establish your reputation, what do you think about collaborating?
Engy Ziedan (EZ): I think being a good collaborator builds a good reputation. I love interdisciplinary work for various reasons. For one I love science, and science comes in all forms. If you ask me, the best of science has come from collaborations. Interdisciplinary work opens your mind to new questions. But there's very little collaboration between economics and sociology, for example, even though sociology is good at coming up with hypotheses and economics is good at empirically testing the validity of those theories.
BE: Susan, you told me that when you were an undergraduate, you double majored in theater and interdisciplinary science, so you’ve been thinking across disciplines for a long time. How does collaboration function in your current work?
Susan Hassig (SH): In public health, the questions we’re trying to answer are complex and multi-dimensional—especially when you’re dealing with interactions of systems that involve humans, animals and pathogens. There’s no one person who can encompass the high level of capacity in all those things simultaneously, and so collaboration and interdisciplinary engagement are central to public health. I would point to what we’re all experiencing with Covid as a key example. We need biologists who understand the virus. We need immunologists to figure out the best strategies to trigger our immune systems. We need experts in communication to translate that information to people, communities, states and countries that need to determine action based on sound information. For me, collaboration and interdisciplinary work is kind of the default.
BE: Is there an expectation you’ll need to compromise, or bracket your own opinions, when you’re working in tandem with other brilliant people who are coming from different disciplines?
DH: I think a lot of this is about having clear expectations about each person’s role from the start. In the case of our project about opening schools, we didn’t know if it was safe. It was obvious we needed someone in education, which was me, and someone who knew health and understood the data and the structures, which was Engy. We realized this was an infectious disease that we were studying, and that we didn’t know anything about infectious disease, and so Susan joined. In this case we all understood our roles almost implicitly from the beginning. We knew our lanes but, ultimately, we were all producing one thing.
BE: Can you tell the story of how this particular study came about?
EZ: Doug had started this initiative where the department would go for a walk every week. He knew I was working on a few Covid-19 projects. During one of these walks, he said he wanted to investigate the effects of closing schools and asked if I wanted to work on it. I was all in. I hunkered down in our spare room throughout Christmas, and we spoke on the phone daily. Six weeks later, we had a paper. In early January, our report was published.
DH: I think the emergence of the project is interesting because it wouldn’t have happened without the walks. This was the beginning of Covid, so everybody was very isolated, and water cooler conversations weren’t happening, so I might have never come to the idea without walking and talking. But I think there’s a larger point here about what Covid did to collaboration. It created collaborations that wouldn't have happened, because of the obvious central problem it introduced, but it also shut down those informal conversations that lead to collaborations.
BE: Susan, what’s the story about how you entered this project?
SH: In the very early phases of the pandemic, Engy and I were trying to understand what could happen. She had some data, and so we talked about modeling it along the lines of influenza to see whether that could give us a reasonable prediction. It didn’t really pan out, but that was the first connection I had to what ultimately became this trio. I think that the defining of roles, having a shared understanding, and being able to let go of egos are important pieces in collaboration. I’m not worried about being a first author at this point in my career, I’m interested in being involved in something that's interesting where I can learn during the process. Learning the jargon and the language of analytic processes and approaches in economics and translating it into the kinds of analytic processes we do in epidemiology and biostatistics was so beneficial for me.
BE: When you say letting go of ego, I am struck by the pressures on undergraduates and their struggle to get into highly selective colleges such as Tulane. How do we emphasize the importance of collaboration to undergraduates, who may inherently lean towards competition?
EZ: I can take a stab at this. I teach an “Introduction to Health Policy” class and an “Introduction to the Pandemic” class. We teach that epidemiology, public health, statistics, and economics are all important, and these classes are a combination of all these components. A professor may be better at one subject, but they are absolutely going to incorporate the thoughts and ideas from other disciplines. Students listen to a variety of seminars, and in doing so they learn how to be open to how other scholars think, and respect people from other disciplines.
BE: One of the most common things students will say after completing a group project is, “I did all the work!” In collegiate settings, the entire group gets an A, but one student may have carried the group. It seems to me in those scenarios that the work may have been good, but the teamwork was poor.
DH: I think that’s part of what’s different about research and collaboration in our fields rather than in a classroom where everybody essentially needs equal credit and an equal-sized role and that’s the way that the grading system works. That’s frustrating to the student that ends up doing the lion’s share of the work. In the case of research, it’s very common to have a few people or just one person who is really taking the lead in the analysis and the writing. The authorship is portioned by how much time people are willing to put in, which, again, is best determined at the outset.
SH: I think we really need to teach students how to collaborate and how to create structures for accountability. I think we assume people already know how to hold others accountable. It’s even more challenging at the student level because they don’t have hierarchical relationships. However, I like to focus on the end result. In some cases, even as a student, if you get a reputation for being a slacker, it spreads and nobody wants to work with you. I think it’s critical to help students understand that collaboration is the norm in almost any effort of major importance. No one can do it all by themselves, and if you don’t pull your weight, then you know that you won’t be there again.
BE: Do you have any innovative pedagogical approaches to teaching these aspects of collaboration?
EZ: Yesterday in class, I had a conversation with a student majoring in public health who said to me, “I’m struggling with my code.” I advised her to get help from an economics student. So now I have two students working together, one from political science and one from public health, and while their common language is the question and the data, what they do with it is very different. I think students conversing via data is driving interdisciplinary work across campus.
BE: What does it look like when people in collaboration are disagreeing? Is this a part of what makes collaboration special, or is that a moment when collaboration fails?
SH: If someone has a divergent opinion, it might be important for the collaborative group to ask, “Why is that divergence occurring?” We might need to step back and check that we’ve really addressed the issue that might be the basis of that divergence. But I think ultimately in a collaborative process, you find the consensus, which might be considered a dirty word right now. You compromise on how to summarize or collectively represent the information you’ve determined. I’ve also never read a research article that doesn’t say more work is needed in some way shape or form.
BE: Did any of you ever disagree in collaboration?
DH: I can’t think of anything where we really disagreed. There was another project I was working on that was just scuttled because we couldn’t agree on certain things. One key thing to remember is that at each point of the conflict, there is learning. It could be that there’s initially a conflict and then you talk through it, and then you realize, “Oh, actually, I just learned something because this other person brought up something.” Then you find a common path forward that’s illuminating and probably better than what you would have done otherwise. In some cases, you don’t really come to that agreement, but you find a way through it.
EZ: My secret wish in life is to collaborate with co-authors in Europe, because then I could keep the paper going 24 hours a day.
DH: We pretty much did that with our paper. I think we took a few hours off, but we wrote in just six weeks!
The Effects of School Reopenings on COVID-19 Hospitalizations
Study Overview
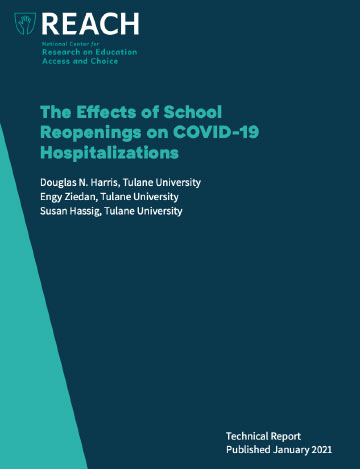
At the onset of the COVID-19 pandemic, we saw a nationwide shutdown of schools that lasted, in many cases, for well over a year. What effect did this extended closure and societal disruption have on COVID transmission and health outcomes? Three Tulane professors decided to try and find out.
In launching their study, Harris, Ziedan and Hassig assembled a unique data set that combined school reopening decisions and health outcomes from essentially every county in the nation. They used the data to compare the health trajectories of districts that reopened in-person earlier in the fall of 2020, with those that remained remote.
They found that counties whose pre-opening COVID hospitalization rates were, per week, below roughly 36-44 per 100,000 people saw no negative health repercussions due to the reopening of in-person learning. As of fall 2020, roughly 75% of the nation’s counties were within this apparent “safe zone.” For the counties where hospitalization rates were above the threshold, the results were less clear cut. For this reason, we concluded that it might be unsafe to reopen during periods of high community spread.
This was the first study to consider the issue on a national basis. Another key advance was their focus on COVID-19-related hospitalizations. Other studies had focused on COVID cases, but Harris, Ziedan, and Hassig explained that the number of observed COVID cases depended on the extent of COVID testing—which itself changed with school reopening. Also, the vast majority of COVID cases are asymptomatic and do not reflect negative health outcomes.
The Centers for Disease Control and Prevention has cited their study more than once as justification for their health guidance. Recently, the CDC has also followed Tulane economists’ lead in emphasizing hospitalizations over cases as the more pertinent factor in decision-making.